Understanding Post-Traumatic Stress Disorder (PTSD)
Introduction
Imagine reliving a terrifying event as if it’s happening all over again. This is just one aspect of Post-Traumatic Stress Disorder (PTSD), a debilitating mental health condition that can develop after exposure to a traumatic event. It affects millions of people from all walks of life, regardless of age, gender, or background. In this comprehensive guide, we’ll delve into the complexities of PTSD, exploring its causes, symptoms, neurological underpinnings, risk factors, protective factors, and evidence-based treatments.
The Prevalence of PTSD
PTSD is more common than you might think. In the United States alone, an estimated 8% of the population will experience PTSD at some point in their lives, translating to approximately 3.6 million adults annually [1]. This staggering statistic underscores the profound impact of trauma on mental health and emphasizes the need for understanding and addressing PTSD.
What is PTSD?
PTSD is a mental health condition diagnosed by a mental health professional that develops after exposure to a traumatic event. These events can range from natural disasters and accidents to war, interpersonal violence, and even witnessing such events. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) outlines specific criteria for PTSD diagnosis, typically categorized into four main symptom clusters:
- Re-experiencing: Flashbacks, intrusive memories, and nightmares can vividly reawaken the traumatic event, inducing intense emotional and physical distress.
- Avoidance: Individuals with PTSD may actively avoid reminders of the trauma, including people, places, or activities associated with the event, in an attempt to escape distressing memories and emotions.
- Negative Thoughts and Feelings: Feelings of guilt, shame, hopelessness, and emotional detachment often plague individuals with PTSD, hindering their ability to maintain positive relationships and outlooks.
- Increased Arousal and Reactivity: Hypervigilance, sleep disturbances, irritability, and exaggerated startle responses are common manifestations of heightened arousal in individuals with PTSD, significantly disrupting their daily functioning.
The Many Faces of Trauma
While PTSD is often associated with combat veterans, it’s crucial to recognize that trauma can stem from diverse experiences. These may include:
- Violent Experiences: Witnessing or experiencing physical or sexual assault, domestic violence, or a violent crime can precipitate PTSD.
- Accidents: Serious accidents, such as car crashes or natural disasters, can induce profound psychological trauma and trigger PTSD symptoms.
- Sudden Loss: The unexpected death of a loved one can shatter an individual’s sense of safety and stability, leading to the development of PTSD.
- Childhood Abuse or Neglect: Early-life experiences of abuse or neglect can lay the groundwork for PTSD, predisposing individuals to psychological distress later in life.
- Complex Trauma: Repeated or prolonged exposure to interpersonal violence, such as abuse or neglect, can have a particularly devastating impact, leading to complex PTSD with a distinct set of challenges.
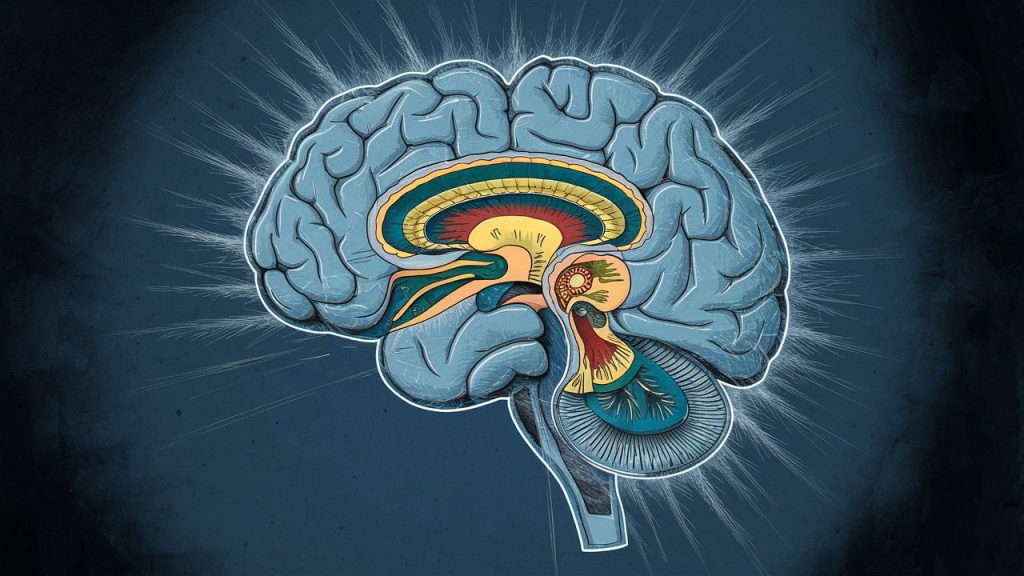
The Science Behind PTSD
The experience of trauma leaves a significant mark on the brain, altering neural circuits implicated in fear processing and memory formation. Key neurobiological changes associated with PTSD include:
- Amygdala Hyperactivity: The amygdala, a brain region central to processing fear and threat detection, becomes hyperactive in individuals with PTSD. This heightened activation perpetuates a state of hypervigilance and contributes to the re-experiencing symptoms characteristic of the disorder.
- Hippocampal Dysfunction: Chronic stress and trauma-related neurochemical alterations impair hippocampal function, compromising memory consolidation and retrieval processes. Consequently, individuals with PTSD may struggle with fragmented or intrusive memories of the traumatic event.
- Prefrontal Cortex Dysregulation: Dysfunction in prefrontal cortical regions responsible for emotion regulation and executive function further exacerbates PTSD symptoms, impairing individuals’ ability to modulate fear responses and regulate their emotions effectively.
Understanding Risk and Protective Factors
While exposure to trauma increases the risk of developing PTSD, several factors influence individuals’ vulnerability to the disorder:
- Severity and Nature of Trauma: The intensity and duration of the traumatic event play a crucial role in determining the likelihood of developing PTSD. Prolonged or repeated exposure to trauma amplifies the risk of psychological distress.
- Genetic Predisposition: Emerging research suggests that genetic factors contribute to individuals’ susceptibility to PTSD, with certain genetic variations influencing neurobiological responses to stress and trauma.
- Early Life Experiences: Adverse childhood experiences, such as abuse or neglect, can sensitize individuals to the effects of subsequent trauma, heightening their vulnerability to PTSD later in life.
- Social Support Networks: Strong social support systems serve as a buffer against the detrimental effects of trauma, promoting resilience and facilitating adaptive coping strategies in the aftermath of traumatic events. Examples include supportive family members, friends, and communities.
Building Resilience: Protective Factors
Several protective factors mitigate the risk of PTSD and enhance individuals’ resilience:
- Resilience: Some individuals possess inherent resilience traits that enable them to cope effectively with adversity and trauma, mitigating the development of PTSD. These traits may include optimism, self-efficacy (belief in one’s ability to cope), and emotional intelligence.
- Positive Coping Mechanisms: Engaging in healthy coping strategies, such as exercise, relaxation techniques (deep breathing, meditation), mindfulness practices, and seeking social support, fosters emotional regulation and resilience, reducing the likelihood of PTSD.
- Early Intervention and Treatment: Prompt access to evidence-based treatments, such as cognitive-behavioral therapy (CBT) and eye movement desensitization and reprocessing (EMDR), significantly improves PTSD outcomes and prevents the exacerbation of symptoms over time.
Conclusion
Post-Traumatic Stress Disorder is a complex and pervasive mental health condition. However, with comprehensive understanding, targeted interventions, and a commitment to healing, individuals with PTSD can embark on a journey of recovery and reclaim their mental well-being. By raising awareness, fostering compassion, and promoting evidence-based treatments, we can empower survivors and create a more trauma-informed world.
Call to Action:
If you or someone you know is struggling with PTSD, there is help available. Please consider reaching out to the following resources for support and information:
- National Center for PTSD: https://www.ptsd.va.gov/
- Substance Abuse and Mental Health Services Administration (SAMHSA): https://www.samhsa.gov/
- MentalHealth.gov: https://www.samhsa.gov/
Remember, healing from trauma is a journey, and you are not alone.